Feeling overwhelmed by persistent skin issues? You're not alone! Understanding fungal acne, a condition often mistaken for traditional acne, could be the key to regaining control of your skin health. Let’s uncover the essential insights you need to combat this frustrating issue.
What You Will Learn
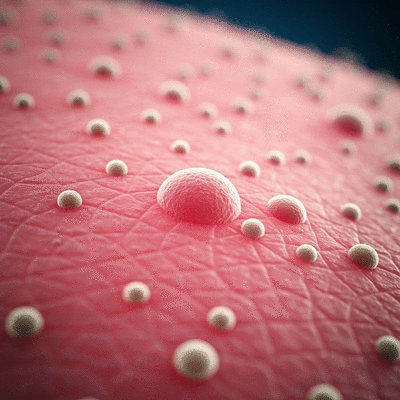
- Fungal acne, or Malassezia folliculitis, is caused by an overgrowth of yeast on the skin, leading to itchy bumps that can resemble traditional acne.
- Common triggers for fungal acne include high humidity, sweating, and the use of heavy skincare products that can disrupt skin balance.
- If over-the-counter treatments fail to improve your skin, it may be time to consult a dermatologist for proper diagnosis and tailored treatment options.
- Patient testimonials reveal that switching to non-comedogenic products and incorporating topical antifungals can significantly improve fungal acne symptoms.
Understanding Fungal Acne Factors and Solutions
This visual outlines the factors contributing to fungal acne and the path to clear skin, including when to seek professional help and real-life patient experiences.
1Causes of Fungal Acne
- • High humidity & sweating
- • Heavy, oily skincare products
- • Antibiotic use (disrupts skin balance)
2When to Consult a Dermatologist
- • Persistent symptoms
- • Increased redness, swelling, pain
- • New or worsening breakouts
- • Signs of infection (pus, fever)
3Patient Experiences & Solutions
- • Maria: Non-comedogenic moisturizer
- • James: Topical antifungal treatments
- • Aisha: Probiotics for skin microbiome
Understanding Fungal Acne: Definition and Causes
Have you ever heard about fungal acne? It's a term that's often misunderstood, but understanding it is key to effective skincare. Fungal acne, scientifically known as Malassezia folliculitis, isn’t your typical acne. Instead, it results from the overgrowth of yeast on the skin, leading to those annoying, itchy bumps you might mistake for regular acne!
At Acne Clarity Hub, I aim to demystify this condition and provide you with the knowledge you need to tackle it head-on. So, let’s dive deeper into what fungal acne really is and what causes it!
What is Fungal Acne? An Overview of Malassezia Folliculitis
Fungal acne occurs when the Malassezia yeast that naturally resides on our skin multiplies excessively. This overgrowth can clog hair follicles and cause inflammation, leading to the appearance of red, itchy bumps. Unlike traditional acne, fungal acne can appear anywhere on the body, but it's most commonly found on the chest, back, and shoulders. Understanding this difference is crucial in choosing effective treatments!
- Malassezia yeast is a part of our skin's natural flora.
- It thrives in warm, humid environments.
- Fungal acne often resembles traditional acne but is caused by different factors.
Recognizing the unique aspects of fungal acne can help you approach treatment more effectively. If you've been grappling with persistent bumps that don’t seem to respond to typical acne treatments, you might be dealing with fungal acne!
Identifying the Causes: Yeast Overgrowth, Malassezia, and Other Skin Conditions
Now, let’s talk about what really fuels this yeast overgrowth. Several factors can contribute to the development of fungal acne, including:
- High humidity and sweating
- Using heavy, oily skincare products
- Antibiotic use, which can disrupt your skin's balance
Each of these factors can create an environment where the Malassezia yeast can flourish. As a board-certified dermatologist, I've seen firsthand how these triggers can compound to exacerbate skin issues. It’s vital to be mindful of your skincare choices, especially if you notice breakouts that don’t respond to typical acne treatments! For more in-depth information on the causes and characteristics, you can refer to resources like this OSU article on fungal acne.
We Want to Hear From You!
Have you ever experienced the frustration of trying to determine if your breakouts are fungal acne or traditional acne? Share your thoughts and experiences below:
Taking Action: Your Path to Clear Skin
Feeling frustrated by fungal acne? You're not alone! It’s important to recognize when it's time to seek help. Sometimes, a little guidance from a professional can make all the difference in your journey toward clear skin.
But how do you know when to consult a dermatologist? There are some key signs to watch for:
When to Consult a Dermatologist: Signs You Should Seek Professional Help for Fungal Acne
- Persistent symptoms that don’t improve with over-the-counter treatments
- Increased redness, swelling, or pain in affected areas
- New or worsening breakouts
- Signs of infection, such as pus or fever
If you're experiencing any of these symptoms, I encourage you to reach out to a dermatologist. My own experience in treating various skin conditions has shown me how vital it is to get the right diagnosis and effective treatment plan tailored for your skin. For further reading on diagnosis and treatment options, consider consulting resources like the National Library of Medicine's research on Malassezia folliculitis.

Patient Experiences: Real-Life Testimonials on Managing Fungal Acne and Effective Treatment
Hearing from others who have faced similar struggles can be incredibly helpful. Here are a few experiences shared by patients who successfully managed their fungal acne:
- Maria, a 24-year-old graphic designer, found that switching to a gentle, non-comedogenic moisturizer made a world of difference for her skin.
- James, a 30-year-old teacher, shares how implementing a consistent skincare routine with topical antifungal treatments helped clear his flare-ups.
- Aisha, a 19-year-old college student, emphasizes the benefits of probiotics in her diet, which she believes helped balance her skin microbiome.
These testimonials highlight the importance of finding the right approach for your individual skin needs. Remember, every skin journey is unique, but there’s always hope for clearer days ahead!
Frequently Asked Questions About Fungal Acne
- Q: What is the main difference between fungal acne and traditional acne?
- A: Fungal acne, or Malassezia folliculitis, is caused by an overgrowth of yeast on the skin, leading to itchy bumps. Traditional acne is typically caused by bacteria, excess oil, and clogged pores, and is not usually itchy.
- Q: What are the common triggers for fungal acne?
- A: Common triggers include high humidity, excessive sweating, and the use of heavy or oily skincare products. Antibiotic use can also disrupt the skin's natural balance, allowing yeast to overgrow.
- Q: When should I see a dermatologist for fungal acne?
- A: You should consult a dermatologist if your symptoms persist despite over-the-counter treatments, or if you experience increased redness, swelling, pain, worsening breakouts, or signs of infection like pus or fever.
- Q: Can diet affect fungal acne?
- A: While not a direct cause, some anecdotal evidence, such as Aisha's experience with probiotics, suggests that balancing your gut microbiome through diet may indirectly support skin health and help manage fungal acne symptoms.
- Q: Are there specific skincare products to avoid if I suspect I have fungal acne?
- A: It's generally recommended to avoid heavy, oily skincare products that can create an environment conducive to yeast overgrowth. Opt for non-comedogenic and lighter formulations.
Recap of Key Points
Here is a quick recap of the important points discussed in the article:
- Fungal acne, or Malassezia folliculitis, is caused by the overgrowth of yeast on the skin, leading to itchy bumps.
- Key triggers for fungal acne include high humidity, heavy skincare products, and antibiotic use.
- If over-the-counter treatments aren't effective, consult a dermatologist for professional guidance.
- Patient experiences highlight the importance of tailored skincare routines and lifestyle adjustments in managing fungal acne.










